On July 1, 2020 we shared a bulletin highlighting the gaps in care related to cancer screenings caused when healthcare systems paused elective and non-emergent exams and procedures in order to preserve capacity in the event of a surge in COVID-19 hospitalizations. The initial bulletin estimated the number of cancer screenings that might be missed and their impact on patient health and costs. Now that more time has passed, emerging data details what has happened.
Epic Health Research Network recently reported that 60% fewer breast, cervical and colon cancer exams were performed nationwide between mid-March and June when compared to the same period last year. The results were similar in Wisconsin: UW Health reported 73% fewer mammograms and 70% fewer colonoscopies when comparing March through June of 2020 to the same period in 2019. Aurora Health Care also postponed mammograms in March, April and early May and saw the number of lung cancer CT screenings decline by 43%.
Getting patients to reschedule missed screenings as soon as possible could save lives and health care dollars. Dr. Ned Sharpless of the National Cancer Institute has cautioned that delayed treatments due to COVID-19 could reverse U.S. improvements in cancer mortality for the first time in more than 25 years. Dr. Harvey Kaufman of Quest Diagnostic, who has researched the decline in cancer diagnosis due to the closure of health care systems earlier this year, predicts that because cancers will be diagnosed at more advanced stages the U.S. will see an excess of 33,890 cancer deaths within the next year.
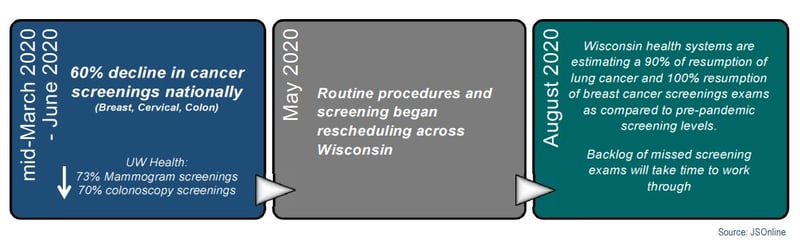
Looking Ahead: The good news is that patients are resuming screening exams. With a backlog of patients due for a screening and extra time allotted between appointments to allow for deep cleaning, it may take a while for the gaps in
care to be closed, which could come at a cost. Oncologists are bracing for an increase in metastatic cancer diagnoses which will require more chemotherapy, radiation, etc. More invasive cancer care is harder on the patient’s body and the chance of recovery is lower than with an earlier diagnosis. Later stage diagnoses are also more expensive. Dr. Federico Sanchez of Aurora Cancer Center estimates that diagnosing lung cancer early in its progression through screening can save $65K over the course of treatment. Offering incentives to encourage team members to re-engage with their health care providers could save lives and improve outcomes.
Sources:
- https://www.jsonline.com/story/news/2020/08/10/cancer-screenings-available-again-but-how-many-cases-were-missed/5532174002/
- https://www.wsav.com/health/covid-19-cancer-dip-in-screenings-could-have-deadly-results/
- https://www.webmd.com/lung/news/20200804/cancer-diagnoses-plunge-as-americans-avoid-screening-during-pandemic#2
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2832226/#:~:text=Average%20total%20cancer%20costs%20were,than%20the%20other%20treatment%20regimens
- https://www.ajmc.com/view/covid19-and-cancer-ncis-sharpless-says-covid-19-could-halt-streak-of-us-cancer-mortality-gains
COMMENTS